I discussed this on our Hockey Physiotherapy podcast. You can listen to that here:
It is always a treat working with teenage hockey players. They have so much going on in their lives - chasing the big league dream, school, their body is changing rapidly and watching them navigate extracurricular’s (relationships, partying) activities etc is always entertaining.
This case I will share today is a knee situation with a young fella - we’ll call him “Johnny”.
He essentially did a million squats, burpees and lunges before a practice one day and it really blew up his anterior knee. He was at another clinic for about 2.5 months and then Johnny’s family checked in with their sports med doc, who then sent him to me.
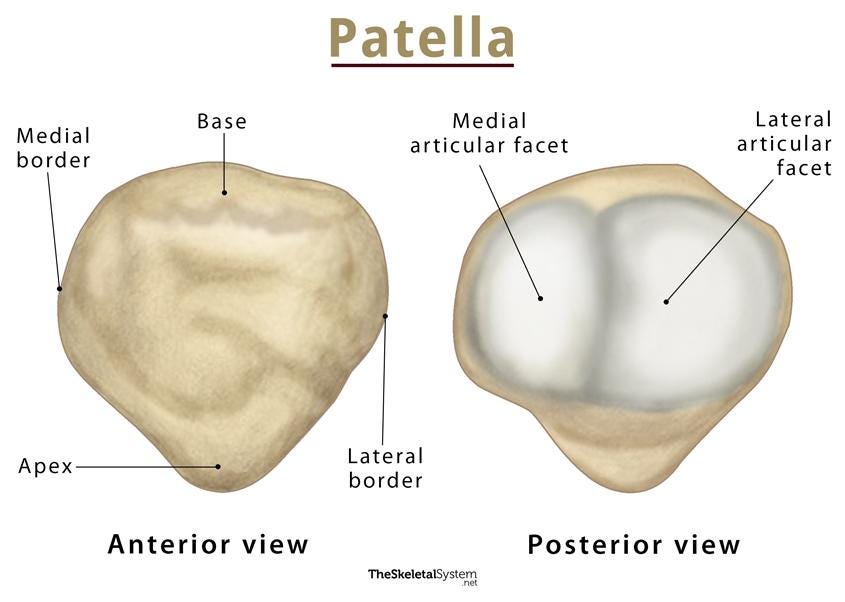
Diagnosis from the sports med doc: tripartite patella (x-ray). Clinically from me: guy had anterior knee pain which seemed to mimic the classic patellafemoral joint issues. Pick your poison on the specific anatomical diagnosis!
We can see anterior knee pain in ice hockey players, but it is not the most common knee injury you’ll see in a hockey player. You’ll see some pre patellar bursa issues from falling onto the knee, however, the most likely knee injury according to Holmes et al. 2018 is an MCL sprain - usually from contact, more rarely is it from catching an edge or something silly like that (15% of the time).
Some newer research by Cattaneo, Ramponi, & Thorborg (2024) would also suggest that of the lower extremities, the knee is the joint most affected by traumatic injuries, while the hip/groin complex is the most affected by overuse problems.
Clinically, on assessment:
Symptoms - stairs were painful, bilateral squatting was 4/10 pain, single leg squatting was 7/10 and sharp deep to the knee cap, walking was fine, he had that classic movie goer’s sign as well where he had anterior knee pain with sitting for longer durations.
Movement was a lot of valgus on squatting movements, lacked understanding on how to hinge, his knee to wall was 3 inches per side restricted in the calf, not ankle impingement so this was an easy red flag for me, pogo hops were tender, a uni lateral hop was even more tender and the pain with these was diffuse below the knee cap. Squat jumps were really provocative. Clarke’s test was positive.
Observation wise: he had 3 cm difference 10 cm above patella, 1.5 cm difference 5 cm above patella. no swelling. I am sure there was some difference there prior to this injury though.
A classic knee PROM/AROM - he was tender in deep knee flexion and lacked knee extension - he was able to get to neutral but when I had em squash the table volitionally with quads he couldn’t get any hyper extension compared to his other side. I measured this with a Goni, of course. I measure everyone’s knee rOM.
I assessed his quad index in sitting at about 70 degrees. He had 40% the quad strength of the other side and it was 3/10 pain. This was obviously one outcome measure. I used LEFS as well. Other outcome measures were simple things like can this dude squat pain free, his knee to wall range of motion, can they lunge pain free, jump pain free etc. The doc also of course ordered imaging because she felt there could have been other things that she was worried about (this was before I saw em).
The beauty of all of this was that it was like mid November and they had a massive gap in their schedule after the first week of December until early/mid January. The family and athlete were cool with shutting down for a bit and then trying to get back on the ice closer to Xmas.
“Partite patella is asymptomatic in most of the patients and usually diagnosed incidentally. It developed due to failure in fusion of accessory ossific nucleus of patella with primary ossification centre in adolescence. This accessory ossific nucleus appears approximately 12 years of age. Patella usually develops from a single ossification nucleus which appears between 3-5 years of age and ossified from centre to periphery. Failure of fusion of these ossification centres may give rise bipartite, tripartite or multipartite patella. Bipartite or tripartite patella becomes symptomatic in young active individuals following direct trauma, overuse, or strenuous athletic activity.” - Faizan et al. 2016
In 2% to 3% of the general population, the finding of bipartite patella on knee radiographs is often incidental as well.
My main goal and outcome measure though was to get him strong and tolerant of a position similar to this:
If I could not get him strong and not in pain a position similar to this prior to getting onto the ice, there was no way, in my opinion, that he was going to have a successful non pain free return to skate. He needed time and strength here before we tried to skate. The musculature needed to catch up to not piss off that joint.
Week 1:
Gave him non provocative strength work for his quads. I have made the mistake before and tried to be aggressive with PFJ and hammer quad stuff through a lot of knee flexion stuff like squats. After making that mistake in the past, I currently approach it more from a straight leg raise vs band perspective, hip lock, leaning tower drills, wall sit variations, high split squat long durations and then going lower variations and then aggressive posterior chain work like RDL’s, hip thrusts, hammy curls with the swiss ball, all of the calf raise variations in the world.
Week 2:
My clinical marker for this athlete this week was pain and full free knee ROM (I was moving him in and out of knee flexion) at 10 days~ post implementation of our exercise plan. I also made us re-check knee to wall, as we know that could impact his knee bending ability. Luckily he was there, but it wasn’t perfect - his squat pain was 0/10 bilaterally, but 2-3/10 single leg - definitely on the right track.
We knew we had a few more weeks before we really needed to get him on the ice.
Single leg squatting was still provocative and I didn’t want to lean into this, but we started doing a ton of band work (at the end of the video) which you can see and watch below on an NSCA video of Mike Potenza.
I gave these to the athlete and had them hammer them daily.
Start of week 3:
We started to do a lot of plyos here and single leg squats became near pain free. So we implemented them 3x a week at low doses.
I knew that once he could tolerate jumps, single leg squats, more extensive plyos/some running that skating should feel fine.
Week 4:
This is where his quad index was nearing symmetry, his LEFs was fine, he could squat, lunge, jump, run, c.o.d pain free.
So I dragged em to the rink and threw em back on the ice similar to this.
No, in reality, I gave em a plan.
Got em back onto the ice at a stick and puck on Monday/Thursday that week and had em wheel around at a hard cap at 15 mins day 1, 20 mins day 2.
No sharp turns, no stops and starts, no skating at above 50% effort. Also, you work with enough kids, athletes, people in general, you learn fast that if you don’t set some guidelines, they are gonna have after and a lot of the time, they still ain’t gonna listen.
Education was really long slow strides, cross overs, c cuts, but not high velocity as better skaters usually have a lower centre of mass - meaning he’d likely be deeper in a squat, as higher caliber players tend to have a wider abduction angle and deeper knee flexion angle. I did not want to over load this too too much.
He had no pain day of or after.
Week 5-6:
Implementation of ice in a team setting - discussion to the coaches saying hey look - this is what he can and cannot do. We started with 20 mins, 35 mins, 50 mins and then full practice. Hard limitations the first week was no hard stops and stops, no battle drills.
This athlete plays for a team that I don’t work with, nor do they have a ton of extra ice access, but if anyone reading this does have more ability to test on ice, then this paper has few ideas which may deem helpful.
Week 7:
Return to play and he did well!
On going:
Educated the patient on his situation, discussed how he still has to keep training, focus on his quad strength, monitor his knee to wall, educated him on anterior knee etc.
I hope this was worth your time reading and any feedback would be greatly appreciated.
The non in text linked references:
Holmes et al. 2018 - https://www.thieme-connect.com/products/ejournals/pdf/10.1055/s-0041-1731795.pdf
Cattaneo, Ramponi, & Thorborg (2024) - https://ijspt.scholasticahq.com/article/90591-what-is-the-injury-incidence-and-profile-in-professional-male-ice-hockey-a-systematic-review
Faizan et al 2016 - https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5018712/